Are you tired of yo-yo dieting?
Are you Looking for Help with an Eating Disorder?
It’s Hard to Find a Trusted Therapist or Counselor to Help with Issues Focused on Food!
Are you using food as a way to fulfill your emotional needs?
- Do you constantly think about food?
- Do you hate the way you look?
- Do you use food to take care of yourself or to punish yourself?
- Are you tired of dieting and don’t know what else to do?
- Body Image Issues?
- Body Shame due to Body Image?
- Do you Feel Guilty Every Time you Eat?

Anne Cuthbert, MA, LPC, LMHC
All Shapes, Sizes & Bodies Welcome!
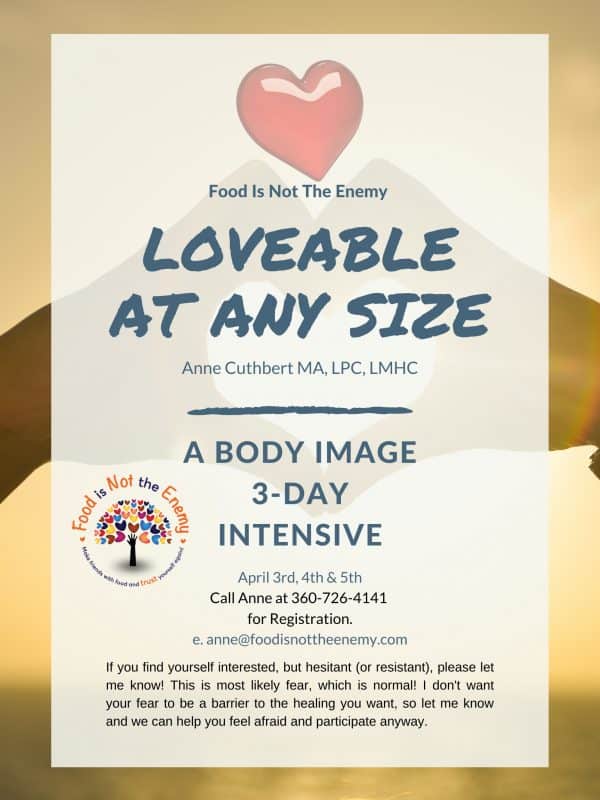
Loveable At Any Size 3-day Intensive Workshop
Date: TBA
Call Anne at 360-726-4141 for Registration.
This workshop is about being open and honest – being your real self, taking risks in a safe environment, deeply connecting with other women, fully receiving acceptance, validation, understanding, value and love from others, healing past traumas / challenges, greater empathy for yourself, letting your emotions out and
more!
And if you’ve done this workshop before, you know how healing it is. Come and do it again for even deeper healing! Really. Each time you participate, you will go deeper and get more healing benefit.
Learn More About the Workshop...We are Growing.
Two New Group Practice Locations to Choose from.
Choose the best location below. We offer all services at both convenient locations.
Careers - Open Counselor Positions for Eating Disorders TherapistsBecause having an eating disorder is a way to cope with emotional challenges, it isn’t uncommon to have Co-Occurring Disorders. What this means is you may be suffering from one or more psychological disorders at one time.
When this other disorder is not properly diagnosed, or addressed, the Eating Disorder can be negatively affected. This can lead to the inability to recover or lead to future relapse. The Eating Disorder can also simultaneously be affecting the other psychiatric disorder, for example, food restriction progressing an anxiety disorder.
Our directory of specialists can help you diagnose and treat the co-occurring problem, in order to successfully rule out the disorder and identify how it is colliding negatively with your current Eating Disorder. You may be curious by now as to what co-occurring issues we are referring to. Here’s a list of one of many that may be harming you and your preexisting Eating Disorder from reaching recovery.
- Depression– effecting 50-75% of Eating Disorder patients, many that may not even be aware. Malnourishment can cause the progression of the patient experiencing super low- lows.
- Anxiety Disorder– affecting 2/3 of society at some point in a persons’ lifetime, ignited by the social anxiety and OCD that may come to the surface with Eating Disorders.
- PTSD (post-traumatic stress disorder)– there has been a higher rate of sexually abused other traumatic events victims and having Eating Disorders. Coming from the feeling of lack associated with coping with the traumatic occurrences, that are often ignored by the fixation the Eating Disorder consumes. This can be diagnosed for anyone who has experienced a traumatic event in their life that has gone improperly treated.
- Substance Abuse– the most common of which are drugs and or alcohol.
- Borderline Personality Disorder (BPD)– this disorder comes with the destruction of the patients’ interpersonal relationships. A need to cope with constant fear of abandonment can lead to an Eating Disorder.
- Self-injury/Self-harm– affecting over 25% of Eating Disorder sufferers, this is often a result of preexisting anxiety, depression and/or trauma and involves the person physically or ritually turning to self-harming physical body tissue in order to relieve the anxiety or overwhelming feelings that come with the illness.
Through treatment for an Eating Disorder, you can also uncover the underlying issues present that co-exist with both disorders/challenges in play. Reach out and tell your story to our group of professionals experienced in the subject of diagnosing Co-occurring issues while having an Eating Disorder. Together, we can help you identify the preexisting issue to keep it from continuing to conflict and or merge with your Eating Disorder.
Reach out to us by phone or email (whichever you are most comfortable with) and we can help you get the help with going forward. When you are ready, look through our directory and find and contact a professional who is well versed with Eating Disorders and understands other mental health challenges. We have provided a directory to help you receive the best possible care to reach recovery and heal your mind in order to heal your body for good! Just one phone call or email away- let’s get started on a beautiful journey towards recovery:)
What is Binge Eating Disorder (BED)
Binge Eating Disorder (BED) is commonly known by compulsive overeating or consuming abnormal amounts of food while feeling unable to stop and a loss of control. Binge eating episodes are typically classified as occurring on average a minimum of twice per week for a duration of six months.
BED was first explained in 1959 by Albert Stunkard, a psychiatrist, and researcher, as Night Eating Syndrome (NES). The term Binge Eating Disorder was created to define similar binge eating behavior without the nocturnal aspect.
Those suffering from BED struggle with emotions of disgust and guilt and often have a related co-morbidity, such as depression or anxiety.
The negative feelings that usually accompany binge eating often lead one to continue to use food to cope; thus creating a vicious cycle. Managed eating disorder treatments are extremely important.
Causes of Binge Eating Disorder
While the exact cause of BED is unknown, there are a variety of factors that are thought to influence the development of this disorder. These factors are:
- Biological: Biological abnormalities, such as hormonal irregularities or genetic mutations, may be associated with compulsive eating.
- Psychological: A strong correlation has been established between depression and binge eating. Body dissatisfaction, low self-esteem, and difficulty coping with feelings can also contribute to binge eating disorder.
- Social and Cultural: Traumatic situations, such as a history of sexual abuse, can increase the risk of binge eating. Social pressures to be thin, which are typically influenced through media, can trigger emotional eating. Persons subject to critical comments about their bodies or weight may be especially vulnerable to binge eating disorder.
Signs & Symptoms of BED
As individuals suffering from binge eating disorder experience embarrassment or shame about their eating habits, symptoms may often be hidden.
The following are some behavioral and emotional signs and symptoms of BED:
- Continually eating even when full
- Inability to stop eating or control what is eaten
- Stockpiling food to consume secretly at a later time
- Eating normally in the presence of others but eating a lot when isolated
- Experiencing feelings of stress or anxiety that can only be relieved by eating
- Feelings of numbness or lack of sensation while bingeing
- Never experiencing satiation: the state of being satisfied, no matter the amount of food consumed
The consequences of BED involve many physical, social, and emotional difficulties.
Binge Eating Disorder Treatment
Professional support and treatment from health professionals specializing in the treatment of binge eating disorders, including psychiatrists, nutritionists, and therapists, can be the most effective way to address BED.
Such a treatment program would address the underlying issues associated, focusing on the central cause of the problem.
It is necessary to concentrate on healing from the emotional triggers that may be causing binge eating, having proper guidance in establishing healthier coping mechanisms to deal with stress, depression, anxiety, etc.
About Food Addiction
There are two main categories of addiction: process addiction, in which a person compulsively engages in behavior(s) that become unmanageable; and substance addiction, in which a person compulsively consumes a substance to the point that they have lost control.
Although drugs and alcohol, for example, can create a physical dependence on the substance, this is not the case with food addiction. No one is addicted to food itself, no matter how much sugar, salt or other the item contains. Instead, an addiction to food is actually an avoidance of emotions. When we avoid emotions, a natural occurrence in all people, we must use something to help us keep the emotions down. For those who use food to do so, food can start to feel like an addiction. However, it is shown that when you let go of food as good or bad and start to eat what your body desires, the “addiction” to food decreases and can completely disappear. Therefore, food addiction is different than substance addiction in this important way. Of course, they share the similarity in that both are used as unhealthy ways of coping with life’s challenges and emotions. This is why therapy can be very helpful for both substance addiction and food “addiction.”
What are the Signs and Symptoms of Food Addiction?
Researchers at Yale University’s Rudd Center for Food Science & Policy developed a questionnaire to identify people with food addictions. The Yale food addiction scale includes the following:
- End up eating more than planned when you start eating certain foods.
- Keep eating certain foods even if you’re no longer hungry.
- Eat to the point of feeling ill.
- Worry about not eating certain types of foods or worry about cutting down on certain types of foods.
- When certain foods aren’t available, go out of your way to obtain them.
- The behavior continues despite negative consequences.
The questionnaire also seeks to ascertained the impact of food on an individual’s personal life by asking if the following applies:
- You eat certain foods so often or in such large amounts that you start eating food instead of working, spending time with the family, or doing recreational activities.
- You avoid professional or social situations where certain foods are available because of fear of overeating.
- You have problems functioning effectively at your job or school because of food and eating.
What Causes Food Addiction?
Those with binge eating disorder (BED), eating disorder-not otherwise specified (ED-NOS), bulimia, a family history of substance abuse, a personal history with substance abuse, or early life trauma are most vulnerable. Often, they have identifiable binge foods such as sugary dessert or salty snack items. Often, they want desperately to stop consuming these foods, but are unable to do so without help. It is not unusual for them to hide food, destroy the evidence such as wrappers, or eat in secret.
Food addiction frequently co-occurs with a mood disorder like depression or post-traumatic stress disorder. Co-occurring dependency on alcohol or abuse of such substances as stimulants, cocaine, marijuana, benzodiazepines, or nicotine is also common
There is nothing bad, wrong, or unhealthy about being fat! Fat is a word that has been vilified by several aspects of culture: media, medical teachings, family members, etc. As a result, people in larger bodies have been made to feel shame about their bodies. This shame starts in early childhood and can be pervasive throughout the lifespan! It’s no wonder eating disorders thrive as people of all gender expressions struggle to fit in with others. This need to “fit in” is based in our survival instincts to be a part of a group. After all, we would survive more readily in a group if chased by a tiger.
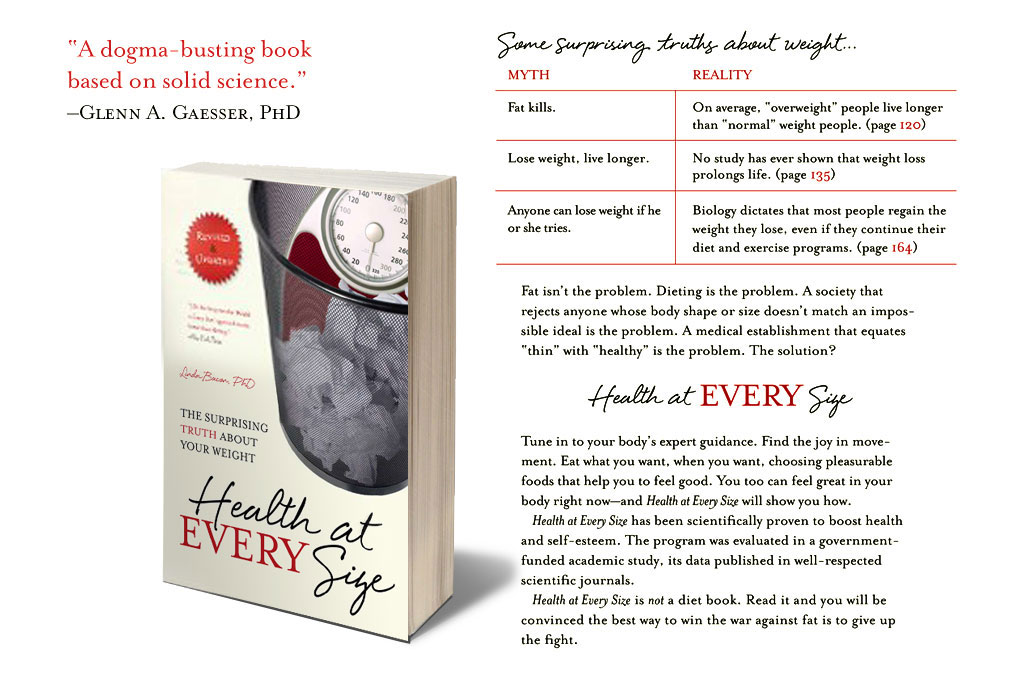
If you are struggling with an eating disorder and feel shame about your larger body, we can help! We can’t change the societal views tomorrow (although things are changing for the better slowly), we can help you accept your body and find loving spaces where you and your body are loved and accepted as is! The shame and pressure to change your body from medical professionals to family members can be better tolerated when you are surrounded by those that accept you. From there, you can learn to let go of the shame and accept yourself. The providers at Food Is Not The Enemy will never tell you to change your body size, will not prescribe a diet, will not shame your body. We come in all shapes and sizes and we appreciate you as you are! We work from a Health At Every SizeⓇ perspective so you can explore your own feelings about your body in a safe space.
Reach out to us by phone or email (whichever you are most comfortable with) and we can help you get the help you need to take control of your body self-love! When you are ready, look through our directory and find and contact a counselor! We have provided a directory to help you receive the best possible care to reach recovery and heal your mind. Just one phone call or email away can be the start of your improved health, mind and life! Call someone today 🙂
Do you find yourself staring at your reflection in the mirror criticizing it up and down or picking out parts to focus your negativity? Do you blame your body for how it looks in the pants you put on that morning? Do you think it’s your fault that your body looks the way it does? Are you constantly trying to or hoping to change your body?
If so, these are all signs that you have poor body image.
Body Image refers to how you view yourself when you look in the mirror or the image you hold of yourself. This includes but is not limited to:
- what you believe about your appearance including memories, assumptions or beliefs you may have subconsciously subscribed to
- how you feel about your body (height, body shape, weight, etc.)
- how you sense/control your body
Your Body Image falls under two classifications and can depend on the state of mind you are in (since it’s not your body changing from moment to moment):
Negative Body Image – embodies not just a state of mind but an overall emotion. This can be to the point of altering your viewpoint on your appearance or what you are actually seeing in your reflection.
Some examples:
- Do you find yourself perceiving parts of your body unlike they actually are?
- Do you view your body as an exception, a cause of your own failures?
- Do you think that only attractive people are well deserving of having the body you want?
- Do you get anxious, jittery or self-conscious about your own body?
- More often than not, do you feel awkward or uncomfortable in your body?
It may be tough to admit to any of the above questions, yet doing so will help you in your journey toward Positive Body Image
The criteria for Positive Body Image is:
- Seeing your body as it really is
- Celebrating rather than shaming your natural body shape
- Placing little importance on your physical appearance, emphasizing more of your character, morals, personality, and overall items and issues important to you.
- Refusing to place heavy emphasis and extra time worrying about food, weight and or calorie intake.
- Overall feeling comfortable and confident in your body.
Poor body image can lead you straight to an eating disorder and can make full recovery from an eating disorder challenging. Because appearance is highly emphasized and specifics of what the right look is are narrowly specified, many people suffer from negative views of their body. Pair this with our natural desire to fit in with others and it’s no wonder that eating disorders and disordered eating and body image are prevalent in our culture.
You are not alone and it is okay to need help with this challenging issue.
Yes, we all have days in which feeling uncomfortable or critical about our body occurs; this is simply the challenge of living in a weight obsessed culture. However, you can develop more positive body image behaviors, develop a level of respect, self care and confidence about your body, and learn to dodge or block out those negative thoughts or beliefs from you and from others.
Find help here from professionals experienced in the subject of body image. Together you can identify aspects of your life that trigger negative body image behaviors and learn how to fully recover from negative body image and an unhealthy relationship with food.
Reach out to us by phone or email (whichever you are most comfortable with) and we can help you get the help you need to beat this, get your life back, and free yourself from the confined chains of self-doubt! Look through the directory and find a counselor, or anyone specialized in body image in particular! Or call us directly and we will connect you with someone who can help! Call someone today!
What is Negative or Distorted Body Image?
Body image refers to how people see themselves. Distorted body image (also called negative body image) refers to an unrealistic view of how someone sees their body. Like eating disorders, it is seen most commonly in women, but many men and gender non-binary folx also suffer from the disorder.
You begin forming your perceptions of your body’s attractiveness, health, acceptability, and functionality in early childhood. This body image continues to form as you age and receive feedback from peers, family member, coaches, etc.
Personality traits such as perfectionism and self-criticism can also influence the development of a negative internalized image of your body.
Signs & Symptoms of Negative Body Image
Symptoms of unhealthy or negative body image may include:
- obsessive self-scrutiny in mirrors
- thinking disparaging comments about your body and frequent comparison of your own shape and size to other people
- envy or a friend’s body, or just as commonly: the body of a celebrity or someone else in the media.
Causes of Negative Body Image
Sometimes body image is negatively impacted by one or more significant events. For example, a gymnast who is continually chided by her coach and fellow athletes to lose a little weight may develop a deeply ingrained and long-standing dissatisfaction with her body, no matter how thin she becomes.
If you are concerned about your body image, here are some questions to ask yourself:
- Is my perception of beauty distorted from years of media exposure that glorifies a very thin ideal that is unrealistic for most people to obtain in a healthy manner?
- Do I find myself regularly criticizing my own appearance?
Causes of Binge Eating Disorder
While the exact cause of BED is unknown, there are a variety of factors that are thought to influence the development of this disorder. These factors are:
- Psychological: A strong correlation has been established between depression and binge eating. Body dissatisfaction, low self-esteem, and difficulty coping with feelings can also contribute to binge eating disorder.
- Social and Cultural: Traumatic situations, such as a history of sexual abuse, can increase the risk of binge eating. Social pressures to be thin, which are typically influenced through media, can trigger emotional eating. Persons subject to critical comments about their bodies or weight may be especially vulnerable to binge eating disorder.
Signs & Symptoms of BED
As individuals suffering from binge eating disorder experience embarrassment or shame about their eating habits, symptoms may often be hidden.
The following are some behavioral and emotional signs and symptoms of BED:
- Continually eating even when full
- Inability to stop eating or control what is eaten
- Stockpiling food to consume secretly at a later time
- Eating normally in the presence of others but eating a lot when isolated
- Experiencing feelings of stress or anxiety that can only be relieved by eating
- Feelings of numbness or lack of sensation while bingeing
- Never experiencing satiation: the state of being satisfied, no matter the amount of food consumed
Binge Eating Disorder Treatment
Professional support and treatment from health professionals specializing in the treatment of binge eating disorders, including psychiatrists, nutritionists, and therapists, can be the most effective way to address BED.
Such a treatment program would address the underlying issues associated with eating habits, focusing on the central cause of the problem.
It is necessary to concentrate on healing from the emotional triggers that may be causing binge eating, having proper guidance in establishing healthier coping mechanisms to deal with stress, depression, anxiety, etc.
What Will You Experience During Eating Disorder Treatment?
Eating disorders are caused by a myriad of challenges, starting in early childhood. The need to belong and feel loved are at the core of an eating disorder. If feeling loved is disrupted enough, through traumas big and small, acute or ongoing, a person can end up feeling a core sense of unworthiness and unlovability. Along comes an eating disorder to help you out! Since being thin equates to lovability in our society, it isn’t hard to wonder why so many struggle with eating disorders. This is why counseling with someone who understands eating disorders and the connection to underlying emotions, is so important. We help you heal from the inside out, using your eating disorder/disordered eating behaviors to help. This helps both the eating disorder and the underlying emotional challenges at the same time. Learning to have emotions that you were likely talked about of expressing, is important to growth and healing. We help you learn to feel again.
When seeking treatment for an Eating Disorder, it’s important to go to someone who understands Eating Disorders. It may be tempting to seek help from a dietitian that may give you the food plan your Eating Disorder seeks or the therapist that doesn’t understand Disordered Eating and may potential encourage weight loss or dieting.
You may need just a therapist or you may need a whole team of support. If you aren’t sure what you need, reach out to one provider in our directory (all providers verified by us work with Eating Disorders) and allow that person to help you decide.
Below is more information about the types of Eating Disorder Specialists and what to look for to help guide you. Please don’t think too much about it and stall your progress forward. The most important step is the first phone call or email.
First, pat yourself on the back right now for taking this huge step toward finding this directory and wanting help!!!
Types of Eating Disorder Specialists
Professionals who specialize in the treatment of Eating Disorders include the following:
- Eating Disorder Therapists or Counselors: These professionals provide therapy sessions of various types, such as individual, groups, family, workshops, couples. Each has a different style and theory base, such as Attachment Therapy, Cognitive Behavioral Therapy or many others. The most important part is that you like the person and believe he/she can help you.
- Registered Dietitians: These professionals specialize in nutrition and will help you create and maintain a healthy, balanced meal plan that supports recovery.
- Eating Disorder Psychiatrists: These professionals prescribe medications and manage drug therapy.
- Physicians who specialize in treating Eating Disorders: These professionals supervise and oversee any medical complications that may have resulted from the Eating Disorder, such as heart conditions, electrolyte imbalances, etc.
What To Look For in an Eating Disorder Specialist
Seeking a specialist who understands, has training in, and may even have personal experience with recovering from an Eating Disorder is important. Not all professionals really understand the complexity of an Eating Disorder. However, the most important aspect to your recovery is finding someone you like and can learn to trust. Here are some other points to consider when speaking with a provider:
- Does the provider primarily treat Eating Disorders and what experience do they have?
- Can the provider help with other co-occurring disorders that might be important for you?
- Is the Eating Disorder specialist accredited or licensed? Degree accreditations/licenses for Eating Disorders therapists and counselors to look for may include an LPC (Licensed Professional Counselor), LMFT (Licensed Marriage and Family Therapist) or LCSW (Licensed Clinical Social Worker). Psychiatrists and physicians should hold a medical degree.
- You may want to work with a provider who is not yet licensed but is working toward licensure under supervision with a provider who is licensed and specializes in Eating Disorders. This can be a good option if you need lower cost counseling as many will offer a sliding fee.
- What is the approach the professional uses? This is often less important than a feeling of trust and safety with the specialist. Yet working with someone who addresses the Eating Disorder in a way that makes sense to you, may be important.
- Does the specialist already work with a team of other professionals who also treat Eating Disorders, such as those mentioned above?
How can a Dietitian
Help You Have a Great Relationship with
Food and Your Body?
A registered dietitian will support and guide you to find helpful and realistic solutions to your food and body image struggles. Whether you are in eating disorder recovery or have struggled with chronic dieting, a dietitian that understands your unique challenges will help you develop a more positive relationship with food and body image. A dietitian can help you follow an Intuitive Eating and Health at Every SizeⓇ framework to help you to:
* Make peace with food and ditch dieting
* Stop the restrict-binge cycle
* Re-learn your internal hunger and fullness cues
* Regain the freedom to include a variety of foods into your life
* Learn how to adequately nourish your body for your unique lifestyle
* Feel satisfied with your meals
* Build trust in your body’s natural ability to self-regulate and maintain a healthy-for-you weight
* Stress less about food and enjoy life more
Working with a dietitian will give you a chance to address food issues directly, to problem solve specific challenges in your relationship with food and guide you in steps toward healthy eating for your body. Paired with counseling, dietetic support with someone who understands your eating disorder, will help you gain ground in your recovery and healing.
Body dysmorphic disorder is a mental health disorder in which you can’t stop thinking about one or more perceived defects or flaws in your appearance — a flaw that appears minor or can’t be seen by others. But you may feel so embarrassed, ashamed and anxious that you may avoid many social situations.
What are the Signs and Symptoms of Body Dysmorphic Disorder?
Body dysmorphic disorder (body dysmorphia) describes a condition where a person can’t stop thinking about one or more perceived flaws with her appearance. The flaw can either be minor or one that is imagined. Seen from an outside perspective, the obsession with these flaws will seem unnecessary or baseless, but to the person, their appearance seems so shameful and distressing that in some cases they won’t want to be seen by anyone.
Body dysmorphia has sometimes been called imagined ugliness. Body dysmorphic disorder is also occasionally referred to as dysmorphophobia, or the fear of having a deformity.
Signs and Symptoms of Body Dysmorphic Disorder Include:
- Preoccupation with physical appearance, similar to anorexia nervosa and bulimia
- belief that one has an abnormality or defect in appearance that makes her ugly
- frequently looking in the mirror
- avoiding mirrors altogether
- believing that others take special notice of ones appearance in a negative way
- frequent cosmetic procedures with little satisfaction
- excessive grooming, such as hair plucking
- feeling extremely self-conscious
- refusing to appear in pictures
- skin picking
- comparing appearance with that of others
- avoiding social situations
- wearing excessive makeup or clothing to camouflage perceived flaws
Signs of body dysmorphic disorder may include obsessive concern over various physical features such as:
- nose
- hair
- skin
- moles or freckles
- acne and blemishes
- baldness
- breast size
- muscle size
- genitalia
What are the Effects of Body Dysmorphic Disorder?
It is not uncommon for a person with body dysmorphia to intensely obsess over her appearance and body image, often for many hours a day. She may seek out numerous cosmetic procedures to try to fix her perceived flaws but will never be satisfied.
A person may change which body feature is the center of focus over time. She may be so convinced about her perceived flaws that she begins imagining something about her body that’s not true, no matter how much someone tries to convince her otherwise. Similar to anorexia nervosa and other eating disorders, the intense subjective and implacable nature of this condition can cause it to be very trying for those close to the person. The intensity of shame and embarrassment about her appearance that body dysmorphic disorder causes cannot be overstated.
What Causes Body Dysmorphic Disorder?
Our image-obsessed culture may contribute to body image fixation, especially if the person has had experiences she perceives as negative about her body or self-image. The constant barrage of unrealistic, idealized physical perfection can be an aggravating factor.
Certain factors seem to increase the risk of developing or triggering the condition, including:
- having biological relatives with body dysmorphic disorder
- childhood teasing
- physical or sexual abuse
- low self-esteem
- societal pressure or expectations of beauty
Body dysmorphic disorder is a serious disease, particularly if it is accompanied by other co-occurring psychiatric or addictive disorders. Like other eating disorders, body dysmorphia is a medical condition that can result in irreversible health complications, including death in extreme cases.
What is Orthorexia?
Orthorexia is a common co-occurring eating disorder. It is characterized by a fixation or desire to eat only “healthy” foods, or to avoid entire food groups. Every person suffering with orthorexia has their own food preferences; foods they will eat and foods that they won’t. Orthorexics feel isolated from or superior to people who may consume a food they they themselves reject. The most common form of orthorexia is an obsession with healthy foods, i.e. never eating foods that contain additives, and planning one’s diet to the extreme to make sure that undesired foods and food groups are not consumed.
What is Anorexia Nervosa (AN)?
Anorexia Nervosa is a psychological and potentially life-threatening eating disorder. Those suffering from this eating disorder are typically suffering from an extremely low body weight relative to their height and body type.
Often referred to as BMI (Body Mass Index) is a tool that treatment providers often use to assess the appropriateness of body weight for an individual struggling with an eating disorder. Additionally, observations of eating patterns, exercise, and personality traits may give indications of an anorexic diagnosis. Those struggling with anorexia frequently fear gaining weight and have a distorted body image. They often believe they appear much heavier than they are.
Atypical Anorexia Nervosa has all the same criteria for anorexia other than a low BMI. Therefore, there are many people in larger bodies that qualify for an Anorexia Nervosa diagnosis. Although this is more readily accepted, it can still too often be missed by professionals. For example, doctors may believe one doesn’t have an eating disorder at all, especially not anorexia, if they are fat. Sadly, many who need support won’t receive it due to this bias.
Additionally, those who suffer from this eating disorder exemplify a fixation with a thin figure and abnormal eating patterns. Anorexia nervosa is interchangeable with the term anorexia, which refers to self-starvation and lack of appetite.
Major Types of AN
There are two common types of anorexia, which are as follows:
- Binge/Purge Type – The person struggling with this type of eating disorder will often purge after eating. This alleviates the fear of gaining weight and offsets some of the guilt of having ingested forbidden, or highly restricted food. The compensatory purge behavior by the individual with Binge/Purge Type anorexia may purge by exercising excessively, vomiting or abusing laxatives.
- Restrictive – The individual suffering from restrictive anorexia is often perceived as highly self-disciplined. They restrict the quantity of food, calories and often high fat or high sugar foods. They consume far fewer calories than are needed to maintain a healthy weight. This is a heartbreaking form of self-starvation.
Though two classifications of this eating disorder exist, both types exhibit similar symptoms, such as an irrational fear of weight gain and abnormal eating patterns.

Causes of Anorexia
It has been said that genetics load the gun and environment pulls the trigger in eating disorders. This eating disorder is based on genetic predisposition, personality traits, and environmental factors.
Examples of environmental factors that would contribute to the occurrence of this eating disorder are:
- The effects of the thinness culture in media, that constantly reinforce thin people as ideal stereotypes
- Professions and careers that promote being thin and weight loss, such as ballet and modeling
- Family and childhood traumas: childhood sexual abuse, severe trauma, neglect, etc.
- Peer pressure among friends and co-workers to be thin or be sexy.
Examples of biological factors include:
- Irregular hormone functions
- Genetics (the tie between anorexia and one’s genes is still being heavily researched).
Anorexia Signs & Symptoms
An individual suffering from anorexia nervosa may reveal one or several signs and symptoms such as:
- Chronic restrictive eating or dieting, beyond the norm
- Rapidly losing weight or being significantly underweight and emaciated
- Obsession with calories and fat contents of food
- Engaging in ritualistic eating patterns, such as cutting food into tiny pieces, eating alone, and/or hiding food
- Continued fixation with food, recipes, or cooking; the individual may cook intricate meals for others but refrain from partaking
- Amenorrhea: an abnormal absence of menstruation, or loss of 3 consecutive menstrual cycles
- Depression or lethargic stage
- Development of lanugo: soft, fine hair that grows on face and body
- Reported sensation of feeling cold, particularly in extremities
- Loss or thinning of hair
- Avoidance of social functions, family, and friends. May become isolated and withdrawn
What is Bulimia?
Bulimia Nervosa is a psychological and severe life-threatening eating disorder described by the ingestion of an abnormally large amount of food in short time period, followed by an attempt to avoid gaining weight by purging what was consumed.
Methods of purging include forced vomiting, excessive use of laxatives or diuretics, and extreme or prolonged periods of exercising. Often, in these binge/purge episodes, a person suffering from this disorder will experience a loss of control and engage in frantic efforts to undo these feelings.
Since they may have bingeing and purging episodes in secret, they are often able to conceal their disorder from others for extended periods of time. Those suffering from bulimia nervosa often utilize these behaviors in an attempt to prevent weight gain, to establish a sense of control, and/or as a means of coping with difficult circumstances or situations.
Described and classified by the British psychiatrist Gerald Russell in 1979, Bulimia Nervosa comes from a Greek word meaning ravenous hunger. If you or a loved one are suffering from this eating disorder, seek professional treatment for eating disorders.
Major Types of Bulimia
There are two common types of bulimia nervosa, which are as follows:
- Purging type – This type accounts for the majority of cases of those suffering from this eating disorder. In this form, individuals will regularly engage in self-induced vomiting or abuse of laxatives, diuretics, or enemas after a period of bingeing.
- Non-Purging type – In this form the individual will use other inappropriate methods of compensation for binge episodes, such as excessive exercising or fasting. In these cases, the typical forms of purging, such as self-induced vomiting, are not regularly utilized.
Causes of Bulimia
The exact cause of bulimia nervosa is currently unknown; though it is thought that multiple factors contribute to the development of this eating disorder, including genetic, environmental, psychological, and cultural influences. Some of the main causes include:
- Stressful transitions or life changes
- History of abuse or trauma
- Negative body image
- Poor self-esteem
- Professions or activities that focus on appearance/performance
Bulimia Signs & Symptoms
An individual suffering from bulimia nervosa may reveal several signs and symptoms, many which are the direct result of self-induced vomiting or other forms of purging, especially if the binge/purge cycle is repeated several times a week and/or day.
Physical signs and symptoms of this eating disorder are:
- Constant weight fluctuations
- Electrolyte imbalances, which can result in cardiac arrhythmia, cardiac arrest, or ultimately death
- Broken blood vessels within the eyes
- Enlarged glands in the neck and under the jaw line
- Oral trauma, such as lacerations in the lining of the mouth or throat from repetitive vomiting
- Chronic dehydration
- Inflammation of the esophagus
- Chronic gastric reflux after eating or peptic ulcers
- Infertility
Signs and symptoms of binge eating and purging are:
- Disappearance of large amounts of food
- Eating in secrecy
- Lack of control when eating
- Switching between periods of overeating and fasting
- Frequent use of the bathroom after meals
- Having the smell of vomit
It can also create problematic strains between the sufferer and family and friends, particularly as the individual has abnormal eating behaviors and/or the avoidance of social activities to engage in binge/purge episodes.
Bulimia Treatment
Since negative body image and poor self-esteem are often the underlying factors at the root of the problem, it is important that therapy is integrated into the recovery process. Bulimia Treatment usually includes:
- Discontinuing the binge-purge cycle: The initial phase of bulimia treatment for involves breaking this harmful cycle and restoring normal eating behaviors.
- Improving negative thoughts: The next phase of bulimia treatment concentrates on recognizing and changing irrational beliefs about weight, body shape, and dieting.
- Resolving emotional issues: The final phase of bulimia treatment focuses on healing from emotional issues that may have caused the eating disorder. Treatment may address interpersonal relationships and can include cognitive behavior therapy, dialectic behavior therapy, and other related therapies.
Don’t delay and risk serious medical complications. Seek out an eating disorder treatment facility in your area.
Binge Eating Disorder Treatment
Professional support and treatment from health professionals specializing in the treatment of binge eating disorders, including psychiatrists, nutritionists, and therapists, can be the most effective way to address BED.
Such a treatment program would address the underlying issues associated with your relationship with food, focusing on the underlying cause of the problem.
It is necessary to concentrate on healing from the emotional triggers that may be causing binge eating, having proper guidance in establishing healthier coping mechanisms to deal with stress, depression, anxiety, etc.
Some of the types of therapy that can be especially helpful in the treatment of BED. These therapies are:
- Cognitive-behavioral therapy (CBT): It can be especially helpful to work on changing thoughts and behaviors around food and body image which brings up the underlying emotions. This helps improve your relationship with food and your body while also supporting healing the emotions and traumas that lead to the eating disorder.
- Interpersonal psychotherapy (IPT): A form of therapy in which the focus is on an individual’s relationships with family members and peers and the way they see themselves. In addition, the relationship with the therapist provides practice and correcting experiences that support improvement in all areas of life.
- Dialectical Behavior Therapy (DBT): A type of therapy that focuses on teaching individuals skills to cope with stress and regulate emotions. This is recommended for those who struggle with a more severe under control over emotions and feelings of abandonment.
In addition to these methods, group therapy sessions led by a trained eating disorder therapist, as well as eating disorder support groups, may also be effective methods of establishing recovery from BED.
Have you ever stopped and wondered how often you are clouded with media telling you to change your appearance, body shape, or overall look in order to be “prettier, thinner, tanner,” i.e. better?
Feeling the obligation to feed into these vicious ways of marketing is an example of Body Shaming. These subliminal and sometimes obnoxiously obvious messages from the media convince you that you must change in order to be “happy” and accepted by others.
It isn’t just the media! Have you been told by your parents, family members or friends that you should do something to change/fix/enhance your appearance? Diet talk is a great example of doing just that.
Do you even use Body Shaming of yourself to connect with others and to feel part of a group?
Some signs of Body Shaming:
- Judging yourself or comparing yourself to others, wishing you were more like them
- Criticizing others’ appearance
- Internally or externally criticizing others without their knowledge
- Judging people based on their physical features
This default to criticize others’ appearance when feeling insecure is certainly not uncommon. This can become the choice of judgement because it is often easier to target yours or another’s physical appearance, something that appears to be in one’s control, rather than admit to what you, yourself, are dealing with emotionally.
You can end Body Shaming and learn to find the positives in your appearance! No matter what your body shape or size, it is possible to accept yourself just as you are! In turn, you accept others too.
Stop the crazy making cycle of hating your body that never leads to self-improvement. Through our directory of professionals who understand the underlying emotions that drive the shame, we can help you:
- identify why you feel inferior/insecure/inadequate
- surround yourself with body-positive/motivating people
- confront/eliminate people that promote body-shaming
- journal/promote aspects of you that you like
Reach out to us by phone or email (whichever you are most comfortable with) and we can help you get the help you need to beat this and fall in love with yourself again! When you are ready, look through our directory and find and contact a counselor, anyone specialized in Body Shaming! We have provided a directory to help you receive the best possible care to reach recovery and heal your mind. Just one phone call or email away can be the start of your improved health! Call someone today
“HEALTH AT EVERY SIZE™ (also known as HEALTH AT ANY SIZE) is a health-centered paradigm that focuses on total health and well-being, not weight. It promotes active living, eating well without dieting, and a nurturing environment that includes respect and acceptance for people of all sizes.”
From: Healthy Weight Network
Like many, I used to think that being fat was unhealthy. I used to think it was my fault when I gained or lost weight. I believed that the BMI determined my level of self-esteem. I thought that my “ideal weight” was something I should be in control over and if I couldn’t control it, something was wrong with me.
No longer!
Katherine M. Flegal, PhD, Senior Research Scientist at the National Center for Health Statistics, CDC, explains, “Although people think there’s all this evidence out there showing a high mortality risk associated with (being) overweight, in fact the literature doesn’t show it.” Far from it. Flegal’s research, analyzing 30 years of actual deaths in the US, corrected an earlier CDC report that indicated severe risks related to (being) overweight. She showed instead that being clinically ‘overweight’ is associated with a lower death rate than so-called ‘normal’ or ‘healthy’ weight. (JAMA 2005;293:1861-1867). It confirmed much earlier research that had been studiously ignored. -Taken from: Healthy Weight Network.
What is the definition of intuitive eating?
Although many claim that food as a drug is equivalent to the brain activation present in cocaine or heroin use, this simply is not proven. Music also stimulates the pleasure centers in the brain but no one has claimed that music is addictive.
It would be much more productive to think of food addiction from the perspective of an emotional addiction or desire to use food to avoid difficult emotions. When the avoidance of these emotions have connections to the past, particularly in childhood, they can be very difficult to handle. Eating can be a way to manage, although in an unhealthy way, with these painful and overwhelming emotions.
Over time, the use of food to avoid and replace painful emotions with the pleasure of eating can become very compelling and eventually lead to feeling increasingly out of control with food. It certainly can have the feeling of an addictive energy. However, the problem is not actually food.
There has been much research and case examples of the importance of and even necessary aspect of utilizing intuitive eating to help with eating disorder recovery.
Intuitive Eating is about learning to listen to your body and to trust it with a variety of food choices. For the person with an eating disorder, this often starts with adding in previously forbidden foods and/or allowing yourself to eat what you want without judgement.
If food addiction, like alcohol or drug addiction were true, this approach would lead further to eating the addictive foods. On the contrary, over time, this instead leaves you with greater choice around what to eat and a greater trust with your body. Almost like magic, you no longer feel out of control with food. Eventually, you will easily choose foods not from a place of punishment but from a place of self-care.
Pair this with working on the underlying emotions that have lead to the disordered relationship with food and recovery can really begin.
Learning to listen to your body and to eat intuitively can be challenging and scary. Facing the fear of weight gain is often a frightening component. If this fear is too great, you may need to work with a professional who can help you confront this fear and other stuffed-down emotions, so you can stop using food to help you cope.
It is possible to trust yourself with food again! Get help today from someone in our directory. Call or email us or a provider that you think can help. It’s okay to ask for help. We understand that it can be scary and we are here to help! Reach out today and start on your path to Intuitive Eating.
Often called “an addiction to food,” compulsive overeating food is used as a placebo to hide or dodge emotions, daily stresses or emotional triggers.
- Do you often eat to a point of no control or no stopping you?
- Do you eat more frequently than normal?
Do you eat alone for feeling ashamed or guilty? - Do you find yourself obsessed with food or weight gain?
- Do you experience a lot of mood swings on a daily/weekly basis?
- Have others commented or brought attention to your abnormal eating behavior/habits?
- Have you missed out on social activities because of body shame or insecurities about your body?
- Do you or your family have a history of dieting?
- Do you eat very little around others and eat the most in isolation?
- Do you believe that your life will “begin” or be better after you lost weight?
- Do you hide or hoard food in odd places?
Do you have a lot of self doubt or self loathing episodes after an eating session? - Do you find that food is your only friend/companion?
- Have you lost your sex drive?
Even though society or loved ones may advise you to fix the problem by beginning to exercise and going on a diet, the problem is not food consumption but the person using food as a coping method for emotions in their life. A person with this disorder may also be a victim of sexual assault, feeling inadequate and therefore filling this void with food consumption. Binging episodes are also used to numb the negative emotions that come with body shame and insecurity.
Even if you are not a survivor of sexual assault, or find yourself with binges even once a week, we are here to help! Together we can help you identify emotions or memories that trigger compulsive eating. Reach out to us by phone or email (whichever you are most comfortable with) and we can help you get the help you eat regularly again! When you are ready, look through our directory and find and contact a counselor, nutritionist or anyone specialized in compulsive eating in particular. We have provided a directory to help you receive the best possible care to reach recovery. Just one phone call or email away can be the start of a new, healthier you-you deserve this! Call someone today 🙂
Food Is Not The Enemy’s Mission is to help you get the support you need to recover from Disordered Eating, Exercising, and/or Disordered Body Image. In the Portland, Oregon area, we strive to employ specialists that understanding your particular struggle and provide you the support services you need. No matter what type of Eating Disorders / Body Image challenges you have, help is available and it’s right in your backyard. It is possible to recover and Food Is Not The Enemy is here to help you get started on your recovery journey today!
Thinking you have an Eating Disorder can bring about feelings of fear and shame. You may feel alone and that no one understands. You may be afraid and ashamed to ask for help. These and any feelings you have are normal! Yet staying alone in your struggle with food and body image is lonely and likely won’t lead to recovery. Instead, get the help and support you need from people who understand!
Perhaps you’re terrified of gaining weight so you significantly restrict calories, even knowing you aren’t taking good care of your body. This might be a sign you have Anorexia Nervosa. Your fear of weight gain drives you to starve your body, to obsess about food and to fear eating most foods. You may have a body weight below what is healthy for you and may also be malnourished.
Paired with Anorexia Nervosa, symptoms derived from Body Dysmorphia, Orthorexia, and/or Excessive Exercise are common.
Body Dysmorphic Disorder is the desire to constantly hide or change your physique because it does not fit internal or external standards. This leads to shame about your body and drives you toward excessive dieting patterns and eventually Eating Disorders like Anorexia Nervosa or Bulimia Nervosa.
When following an eating lifestyle that thrives off keeping track of ingredients and isolating yourself to only consuming healthy/clean foods, Orthorexia can be an easy disorder to adapt. Orthorexia is about controlling your weight and health and can become increasingly obsessive. Although not an official psychological disorder, insisting on these eating patterns can lead to the same obsessions about food and weight, and shame when you are unable to maintain your restrictive eating.
Perhaps you use Over-Exercising to purge “bad” eating or to control Binge Eating. As well, setting unrealistic goals that exceed healthy exercise can lead to obsessive Over-Exercising. Because coping in this way cuts you off from being able to listen to your body, injury and increased obsession will often result.
When addressing treatment for Anorexia Nervosa (or any Eating Disorder) you will likely grow even more fearful of weight gain, and claiming treatment is not necessary because Anorexia Nervosa is simply a lifestyle, not an illness. You may be ultimately attempting to prevent the effects of body shame that can mentally prolong even after physical recovery and likely began before anorexic behaviors took place.
If you struggle with Bulimia Nervosa, you are likely vomiting or exercising to “get rid of” any amount of food that you feel uncomfortable eating. It may follow a feeling of being too full or it may be that you are afraid of digesting what you did eat. Binge Eating is common for someone with Bulimia Nervosa. Sometimes the binge is eating hundreds or thousands of calories all at once but it doesn’t have to be. Bulimia Nervosa is indicated by the way you get rid of the food, often with vomiting / purging. Those with Bulimia Nervosa come in all shapes and sizes and, like other Eating Disorders, you fear weight gain.
Although a newly diagnosable Eating Disorder, Binge Eating has been around a long time. Most of those with an Eating Disorder struggle with Binge Eating; it’s the most common. Those who binge eat find food soothing and will often turn to food to manage anxiety, depression, loneliness and other emotions. You may or may not exercise to manage the Binge Eating consequences but you likely feel ashamed of eating and try to diet to get back on track.
If you believe you have a Food Addiction, you may have first attempted to get help by avoiding sugar, flour, or other foods you think are driving your addiction. Unlike avoiding alcohol, which is not needed for survival, this tactic will not work with food. In fact, avoiding foods may lead you straight into an Eating Disorder, if you aren’t already struggling. However, your emotions may be the reason you think you’re addicted to food. Using food and hating your body to help you avoid what you’re really feeling is very common.
Each of these patterns of disordered eating lead to feelings of shame about your Body Image. As well, shame about your Body Image can lead you into Disordered Eating. The two go hand-in-hand. Body shame, or not looking the way society or even your parents told you was good enough, is so common in our culture that it may be difficult to spot until your obsession and negative feelings about yourself and your body interfere with your pursuit of happiness and joy.
Recovery from Eating Disorders and poor Body Image are about the practice of viewing food as a vital energy source, and less of a reward or sinful aspect of life and a way to avoid the difficulties of life.
If you think you may have one of the above Eating Disorders, is it possible to get better? Absolutely! We are committed to helping you find the help you need to get out of your Eating Disorder and back into your physically and emotionally healthy life! We can help you because we understand and know the way out.
If you aren’t sure what type of help you need, read more of our articles, call or email us. You don’t have to figure it out on your own! Let us help you. All it takes is a phone call or email to get your started.
What is Exercise Resistance
Do you enjoy exercising? Do you have a physical activity that you just love and can’t wait to do? Or, do you wish you wanted to exercise – after all it will help you lose weight – but you can’t seem to get yourself to do it? Perhaps you yo-yo exercise – you exercise for a while and then, suddenly, you can’t bring yourself to go to the gym or jump on your bike again?
Many people have heard of compulsive (or addictive or over-) exercising. This is a term used to describe someone who exercises too much and/or too often. For many who use compulsive exercise, it is a way to cope with feeling too full or as a way to control weight gain or to compensate for other areas where they feel out of control.
On the other end of the continuum is Exercise Resistance. Francie White, a dietician working with eating disorders in the Santa Barbara California area, coined the term Exercise Resistance. Although it is not widely recognized as a type of eating disorder or body image issue, it is an important element to be explored.
Most of the women who have a resistance to exercise also tend to be emotional eaters, have a history of dieting and/or challenges with body image. Therefore, motivational strategies to encourage exercising fail and the thought of exercising is met with feelings of anger, anxiety and, well, resistance.
What are the risk factors?
- A history of chronic dieting. Resisting exercise may be a way to consciously or unconsciously respond to society’s emphasis on the ideal body as thin… as if to say, “I will not look the way you want me to look!”
- Parents who forced or overemphasized exercising as a way to encourage their child to lose weight. Physical activity stops being play and becomes work and something to dread.
- A history of sexual abuse for women or early onset puberty/development of large breasts. The sexual abuse could have occurred at any age or in any form and may even have occurred shortly after weight loss. In these cases, you may be attempting to prevent sexual attention or intimacy as a larger body size often receives less unwanted sexual attention.
Do you think you have Exercise Resistance?
If you resist exercising, you may want to explore the underlying reasons for this. Remember, it may be more than just finding a coach to help motivate you. You may need to further explore your feelings about exercise and your body.
Would you say that exercise is the most important aspect of your day?
Do you use exercise to control your body shape and or weight?
Do you workout even when you are stressed, ill or in poor weather conditions?
Have you ever missed any school, work or social obligation times for exercise?
If you find yourself saying “yes” to any of these questions, you may be engaged in Excessive Exercise, a disorder that can become addictive. Excessive or Over-Exercising is characterized when the exerciser abuses the frequency, intensity of exercise and makes it his/her top priority. This behavior can fall under many classifications such as:
- Exercise Addiction
- Obligatory Exercise
- Compulsive Athleticism
- Compulsive Exercising
- Exercise Abuse
Other Symptoms/Behaviors
- Get extremely depressed or frustrated when exercise is not achieved, or exercise does not receive that excrete “high”
- Exercise alone to avoid attention from others such as trainers, other people at the gym, etc.
- Always following the same strict exercise schedule
- Exercising for 2+ hours daily, repetitively
- Obsession with weight loss/calories expended
- Exercising past the point of discomfort or pain
In addition, this disorder can be a product of Anorexia Nervosa when used in conjunction with striving for thinness by starvation or with Bulimia Nervosa when it is used to purge calories consumed.
Even if you have a semi positive body image, there is still the possibility of experiencing Excessive Exercise Disorder or behaviors where exercising becomes an obsessive task for the sake of exercising.
You are not alone in this! Through our directory of professional providers, you can help realize the psychological torment and damage of overall wellbeing that comes with the disorder. You can learn other, more effective ways to relieve overwhelming emotions of anxiety that go beyond working out.
Get help from professionals experienced in the subject of Excessive Exercise who can help you identify aspects of your life that trigger your need to burn calories and the shame you feel if you cannot or do not choose to that day. Reach out to us by phone or email (whichever you are most comfortable with) and we can help you get the help you need. Just one phone call or email away can be the start of your improved health, both physically and emotionally! Reach out today!
Men and Eating Disorders: A Widely Ignored Subject
The vast majority of education about eating disorders is focused on women. Admittedly, women are twice as likely to develop an eating disorder due to oppressive societal standards. However, male eating disorders are just as dangerous and far less discussed.
Though men are less likely to develop one of these disorders, it is important to include men in the discussion. About 10 million men in America will develop an eating disorder each year. That’s plenty of risk, warranting an education for both men and women when it comes to these life-altering mental illnesses. Here are a few things to know about men and eating disorders.
Men Can Have Negative Self-Image
Though women receive the brunt of societal expectations, men also receive pressure to be strong, masculine, muscular, and emotionless. Being fit is commonly considered mandatory for male attractiveness. Since “thin” and “fit” are often incorrectly viewed as synonymous, men can easily fall prey to an eating disorder in an attempt to look more fit and, therefore, more attractive.
Men Suffer From Binge Eating Equally as Often as Women
Of course, not all eating disorders cause weight loss. Binge eating has been shown to be roughly as common in men as in women. This disorder falls under the category of “subclinical,” meaning it is not considered severe nor will it result in death.
Anorexia and bulimia are considered clinical as they can cause permanent damage and even death. In studies of subclinical disorders, men actually fall equal to women whereas clinical disorders are more common in women.
Though subclinical disorders such as binge eating are not technically dangerous, they can certainly cause a slew of health problems and often tell of a much deeper issue. Do not ignore binge eating if you see the signs in a loved one. Seek help.
Males Face Additional Stigma and Often Go Untreated
Eating disorders are often associated with women who want to lose weight. While women do face a stigma thanks to misconceptions and misinformation about eating disorders, men have great difficulty. Not only will others believe that they have done this to themselves and just need to stop, but they will also be ridiculed for behaving like a woman.
These two hardships men with eating disorders face can result in undiagnosed disorders and lack of treatment. With the potential fatality of some eating disorders, these stigmas are much more harmful than one might think.
Men are too often left out of the conversation on eating disorders. They have been viewed as a women’s problem and little more than an effort to lose weight when in reality, eating disorders can affect anyone and are typically the result of an underlying issue.
Of course, societal standards on appearance do not help the problem nor does the lack of education the public has on eating disorders. If you notice a male loved one avoiding food, purging, or binge eating, do not shrug it off. With 10 million men a year falling prey to eating disorders, it is not unlikely that your loved one needs help.
Eating Disorder Counselors
NOW ACCEPTING INSURANCE
Bi-Lingual Therapists Available
We are now accepting insurance, including Oregon Health Plan.